Teen Anxiety Treatment: Student Profile
Adolescents who suffer from anxiety may manifest their struggles in a variety of ways. However, parents seek our specialized approach, because your child has been struggling in many of the following ways:
- School Refusal
- Social Isolation
- An inability to complete assignments or responsibilities required for daily life.
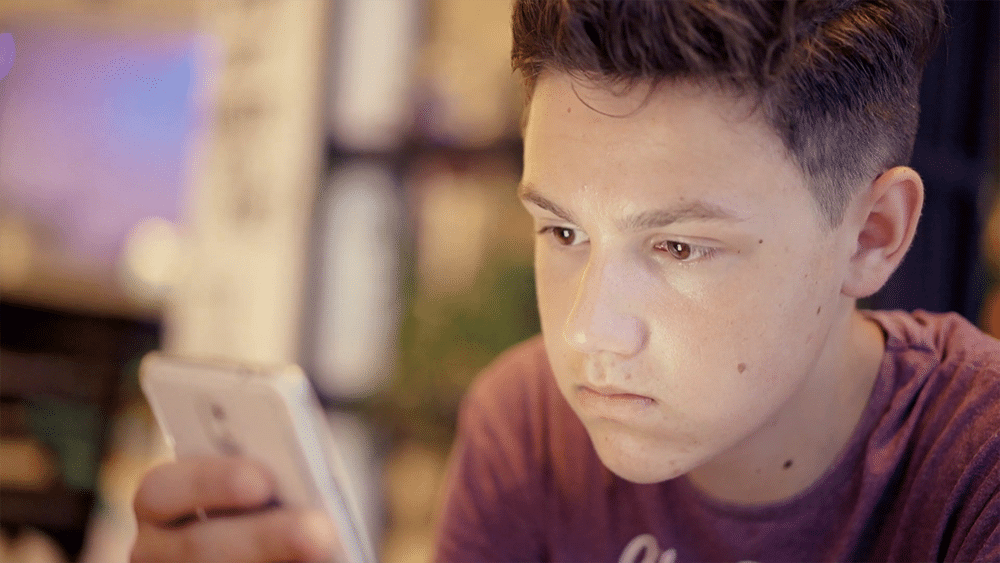
- Living vicariously through social media
- Using “screens” to escape or avoid.
- Skill deficits in the areas of:
- coping skills
- self-advocacy
- problem-solving
- communication
- and frustration tolerance
- Executive deficits in the areas of:
- task initiation
- staying focused
- goal-directed perseverance
- and emotional control
(click below to go to a section on this page)
- How your child appears to others outside of the home can be dramatically different from the behaviors exhibited within the home, particularly when your child’s avoidance is being challenged (i.e. “It’s time to turn of the computer”).
- Tantrums aimed at getting others to accommodate them.
- Physical complaints, including G.I distress, illness, migraines, etc.
- Sensitivity to noise volume, foods, textures, etc.
Students enrolled at WayPoint Academy are not “troubled youth” as their admissions are not due to natural consequences of prolonged misconduct. On the contrary, teenagers who suffer from severe anxiety often spend considerable energy to appear “normal” to the outside world. Often, friends and relatives of the family are surprised to hear that the child is struggling, and that parents are pursuing a residential level of care.
What Anxious Teens Have in Common: Maladaptive Coping Strategies
Thorndike's Law of Effect posits that humans are hardwired to seek pleasure and avoid pain. To help avoid the pain that comes with anxiety, teens often develop negative coping mechanisms to get out of situations that may be stressful.
These maladaptive behaviors prevent your teen from adapting to new or difficult circumstances. Maladaptive coping strategies are not only unhelpful, they negatively impact your teen’s mental well-being. Such behavior prevents them from engaging in stressful situations – mentally, physically, or emotionally – and can lead to social isolation.
When teens avoid situations, events, and people, they can damage their development, restrict their growth, and fail to meet their psychological needs. Anxiety-provoking situations increasingly feel out of control and painful to think about, so teens rely on and strengthen their negative coping strategies, creating a negative feedback loop. Eventually, they even start missing out on activities and relationships they enjoy.
“Problems are not the problem; coping is the problem.”
- Virginia Satir, a prominent clinical therapist
Avoidance
Teenagers who deal with severe anxiety are often “white knuckling it” during the day -- displaying polite, helpful, and compliant behaviors. Yet at home, they struggle with emotional control and can exhibit disruptive behaviors, particularly when their avoidance is challenged i.e. (“It’s time to turn off the computer” or “You need to do your homework”). When avoidance is challenged at home, it is not uncommon for the child to use behavior as a negotiating tool to get their parent to accommodate, by giving them what they are seeking or to remove or ignore certain obstacles that are anxiety-provoking.
A common denominator for nearly all who struggle with severe anxiety is avoidance. Avoidance may be manifested in the overuse of digital media/video gaming, social isolation, psychosomatic complaints, overly critical judgments of others as a means of justifying isolation, self-sabotage, and a myriad of other maladaptive behaviors. Such avoidance further contributes to one’s inability to function adequately at home, in the community, and in traditional school settings. Due to the level of avoidance that has taken place over time, these youths lack the necessary skill development that will empower them to overcome the challenges of life.
Life-interfering Behaviors & Effects of Anxiety
The main difference between the everyday worry that teens experience and clinically diagnosed teen anxiety, is the level to which anxiety affects your teen's life. One of the most common ways anxiety affects our students' lives is in the area of social practice and learning.
Social Practice & Learning Deficits
Social practice is a crucial part of teen development. Social settings are where we learn how to have relationships with others, build self-confidence and develop the ability to complete daily tasks at work or school. While new social interactions are often “awkward” for most people, they can be excruciatingly painful for teens with anxiety. However, social practice exposes teens to:
- new ways people pursue and overcome various challenges
- new possibilities for action as they practice social skills in different social settings
- appropriate responses as they experience the stresses of different social settings
Even short periods of time without social practice and learning can affect teen development. If your teen also struggles with anxiety, periods of isolation or remote learning may have long-lasting effects that need a focused effort to overcome.
Persistent Pattern of Not Completing
Anxious teens have a pattern of not just avoiding, but they’re also not completing things in their lives. Their anxiety prevents them from getting from point A to point B in most aspects of their life. You can notice this pattern any time they say “I wanted to ______, but couldn’t.”
For example, they may say:
- “I wanted to join that club, but just couldn’t.”
- “I wanted to try out for that play, but couldn’t.”
- “I wanted to ask that person on a date, but couldn’t”
- or “I wanted to turn in my completed assignment, but couldn’t”
What's left unsaid, is that they couldn’t accomplish something they desperately wanted because their anxiety overwhelms every other desire.
Completion is the antithesis of avoidance. Strength and empowerment come from facing and completing challenges, and as your teen mindfully addresses the source of struggles, they gain experience, confidence, and emotional endurance.
Compulsive Need for Accommodations
Adolescents with severe anxiety do not suffer alone. Inevitably, the whole family is affected. Many parents recognize the symptoms of anxiety and their accompanying avoidant behaviors, yet feel powerless in bringing about positive changes. Parents often become overwhelmed by their child’s disorder, and develop patterns that accommodate avoidance in order to further avoid significant family conflicts. As a result, the external environment frequently adapts to the needs of the teen—at the expense of the youth learning to adapt to the demands of the world.
Family participation is essential in the healing process. Through family therapy, parent visits, and seminars, WayPoint Academy directs families toward making adjustments and changes to support their student’s progress.
Getting to the Root of What's Causing Your Teen's Anxiety
Everyone experiences anxiety to some degree. Worrying about certain situations like exams, job interviews, and romantic relationships is normal. But when a teen’s anxiety starts to interfere with everyday life, or when it becomes chronic and debilitating there are two common causes:
- there is an underlying cause, experience, or environmental factor that contributes to a teen’s anxiety.
- a teen has an underlying genetic predisposition for anxiety.
Underlying causes, experiences, or environmental factors contributing to anxiety in teens
Everyone has anxiety to some degree or another. The question is how much does it impact your life? Sometimes there are behaviors and situations that can increase your anxiety to the level of needing treatment. These may include:
- technology overuse and addiction
- deteriorating relationships with friends or family members
- substance abuse
- experiencing a traumatic event
- moving to another city or away from a support network
- having a learning difference
In these situations, if you treat the underlying problem, the anxiety will often become manageable or disappear altogether.
Standard therapy approaches like CBT and ACT can help these teens with anxiety.
Teens with an underlying genetic predisposition for an anxiety disorder
When someone struggles with acute anxiety or an anxiety disorder, often the anxiety is at the root of problem behaviors rather than a result of them. For these teens:
- these teens have struggled with anxiety their whole life and their anxiety is not a result of a specific event, situation, or behavior
- their anxiety does not get better if they stop problematic behaviors such as technology use. Often their anxiety gets worse
- these teens will always have anxiety throughout their life. The goal is not to make the anxiety go away, but rather equip these teens with the skills necessary to be able to manage their anxiety throughout their life to prevent it from significantly impacting their life
- they need a therapeutic approach that has been specifically designed for treating acute anxiety in teens, and for healing teen anxiety disorders. Therapeutic modalities like Exposure Therapy (ERP).
WayPoint's Treatment Program Helps ALL Teens Suffering From Anxiety
The good news is that regardless of what is causing your teen's anxiety, WayPoint can help. The essence of our specialized psychotherapeutic approach is in finding the right model for each individual student and matching it with the right intervention. Our teenage anxiety rehab program is designed to provide a host of therapeutic assignments and tasks that are designed to increase distress tolerance and emotional resiliency in teens with all types of anxiety.
Types of Teen Anxiety Disorders WayPoint Academy Can Help
Generalized Anxiety Disorder
Generalized Anxiety Disorder (GAD) is characterized by excessive, uncontrollable, and often irrational worry about everyday things that is disproportionate to the actual source of worry. It's normal to feel anxious from time to time, especially if an individual’s life is stressful. However, severe, ongoing anxiety that interferes with day-to-day activities may be a sign of generalized anxiety disorder. These excessive worries often interfere with daily functioning. Individuals suffering from GAD typically anticipate disaster and are overly concerned about everyday matters such as health issues, death, family problems, friend problems, or relationship problems.
Individuals often exhibit a variety of physical symptoms, including fatigue, fidgeting, headaches, nausea, numbness in hands and feet, muscle tension, muscle aches, difficulty swallowing, bouts of difficulty breathing, difficulty concentrating, trembling, twitching, irritability, agitation, sweating, restlessness, insomnia, hot flashes, rashes, and inability to fully control the anxiety. Living with generalized anxiety disorder can be a long-term challenge if untreated.
Anxiety disorders affect 1 in 3 teens
between 13 and 18 years old. Research shows that untreated teenagers with anxiety disorders are at higher risk to perform poorly in school, miss out on important social experiences, and engage in substance abuse.
At least 1 in 200 kids & teens have OCD
This is about the same number of kids who have diabetes.
Obsessive-Compulsive Disorder (OCD)
Obsessive-Compulsive Disorder (OCD) is an anxiety disorder characterized by unreasonable thoughts and fears (obsessions) that leads to repetitive behaviors (compulsions). With obsessive-compulsive disorder, a person may realize that his/her obsessions aren't reasonable, and may try to ignore them or stop them. But that only increases the distress and anxiety. Ultimately, the individual feels driven to perform compulsive acts in an effort to ease stressful feelings.
Obsessive-compulsive disorder often centers on themes, such as a fear of getting contaminated by germs. To ease contamination fears, an individual may compulsively engage in hand washing until they are sore and chapped. Despite the individual’s efforts, thoughts of obsessive-compulsive behavior keep coming back. This leads to more ritualistic behavior — and a vicious cycle that's characteristic of obsessive-compulsive disorder.
Social Anxiety
Social Anxiety (also sometimes called social phobia) is typified by extreme feelings of shyness and self-consciousness build into a powerful fear. As a result, a person feels uncomfortable participating in everyday social situations. People with social anxiety can usually interact easily with family and a few close friends. But meeting new people, talking in a group, or speaking in public can cause their extreme shyness to kick in. With social phobia, a person's extreme shyness, self-consciousness, and fears of embarrassment get in the way of life. Instead of enjoying social activities, people with social anxiety might dread them — and avoid some of them altogether.
Panic Disorders
Panic Disorder is an anxiety disorder characterized by recurring severe panic attacks. It may also include significant behavioral change lasting at least a month of ongoing worry about the implications or concern about having other attacks. The latter are called anticipatory attacks. Panic attacks can be very frightening. When panic attacks occur, an individual might think he/she is losing control, having a heart attack, or even dying. An individual may have only one or two panic attacks in a lifetime, but if having several panic attacks and having spent long periods in constant fear of another attack, such an individual may have a chronic condition called panic disorder.
Agoraphobia
Agoraphobia is a type of anxiety disorder in which an individual is avoiding situations that he/she is afraid might cause a panic attack. People with agoraphobia avoid being alone, leaving their homes, or any situation where they could feel trapped, embarrassed, or helpless if they panic. People with agoraphobia often have a hard time feeling safe in any public place, especially where crowds gather. The fears can be so overwhelming that some people may be essentially trapped in their own homes. Although mostly thought to be a fear of public places, it is now believed that agoraphobia develops as a complication of panic attacks.
2.4% of adolescents have agoraphobia
at some time during their life and all of them experience severe impairment.
Anxiety & Co-occuring Disorders
When a person experiences two or more illnesses at the same time, those illnesses are considered “comorbid.” Some estimates show that 60% of those with anxiety will also have symptoms of depression or another comorbid mental health struggle like ADHD, Autism Spectrum Disorder (ASD), or learning differences.
One-third of substance abusers struggle with comorbid anxiety
Reciprocally, one-third of people with anxiety abuse substances.
